Page Summary:
While some surgeries carry a risk of harm, abortion is intended to harm. It may be one of the most common surgical procedures in the world, but it is hardly a harmless one. A better understanding of the techniques involved makes this abundantly clear.
Primum non nocere! This Latin phrase meaning "First, do no harm" is one of the principal precepts guiding all medical intervention. Like the Hippocratic Oath, which also vows to "never do harm," it is a reminder that the physician's role is to heal, not to harm. While many surgical procedures carry the risk of harm, their intent is to provide healing for the patient. The explicit intent of abortion, however, is to harm the embryo or fetus to death. Abortion may be common, but it is by no means simple or benign. From an ethical standpoint, it results in the violent destruction of a living human being. From a technical standpoint, abortion is usually a blind, surgical procedure that takes place within one of the most vulnerable regions of a woman's body. Prominent abortionist, Warren Hern, has literally written the book on abortion (Abortion Practice), and he speaks of it as such:
One of my more experienced colleagues recently commented, “Abortion is a simple procedure except for the uterus’s total intolerance to poor technique.” The first half of this comment summarizes the popular notions about abortion within the medical community; the last half summarizes the wisdom of one who is experienced with the pitfalls of this “simple” procedure. In medical practice, there are few surgical procedures given so little attention and so underrated in its potential hazard as abortion.
No matter how much "relief" abortion provides for the mother who doesn't want a baby, it is a procedure that violates the most basic medical ethic. Listed below, you will find information on the various methods used to "abort" a developing embryo or fetus—including suction curettage (vacuum aspiration), oral medication, dilation and evacuation (D&E), and dilation and extraction (D&X or partial-birth abortion). Remember that these are descriptions of legal medical procedures designed to kill living human beings who have given absolutely no consent to be terminated.
Suction Curettage or Vacuum Aspiration Abortion:
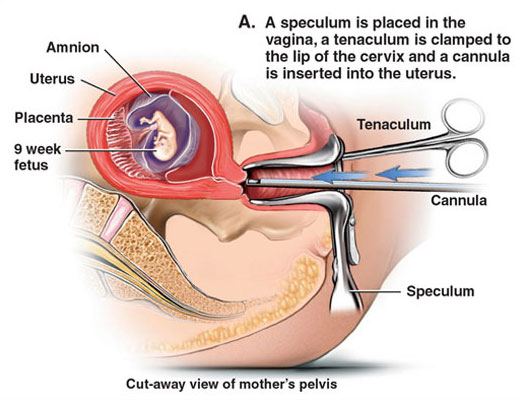
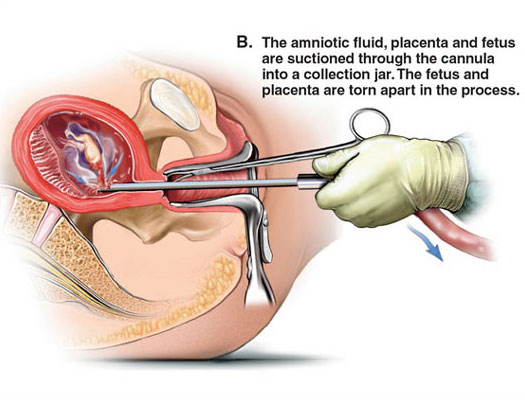
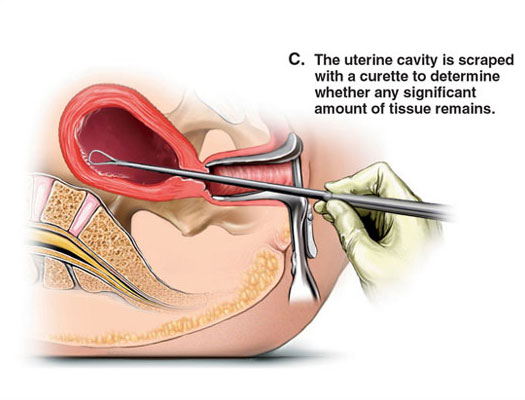
MEDICAL ILLUSTRATIONS OF A SUCTION CURETTAGE ABORTION (click images to enlarge)
Copyright © Nucleus Medical Art, Inc. All rights reserved. www.nucleusinc.com
Suction curettage abortion (also called vacuum aspiration) is the most common abortion procedure in the world. It falls under the broader banner of dilation and curettage (D&C), which can also be performed with a sharp curette. Suction curettage was first used in Russia in 1927.2 Thirty years later, the technique was "perfected" in China.3 Today, the National Abortion Federation (NAF) reports that "virtually all modern first-trimester surgical abortions are accomplished by vacuum aspiration."4 In 2015, roughly 73% of U.S. abortions were performed surgically,5 and 86% of these were performed at or before 13 weeks gestation.6
Most suction procedures begin with anesthesia. According to the NAF, "where deep sedation or general anesthesia is not used, the patient may need preparation time to learn strategies to manage her anxiety before the procedure starts."7 A 2002 NAF survey indicates that 46% of U.S. providers prefer cervical anesthesia, 33% prefer a combination of cervical anesthesia with IV conscious sedation, and the remaining 21% prefer deep sedation or general anesthesia.8 Though the use of general anesthesia is considered safer than it was when Warren Hern first published his textbook on abortion, he advises against the practice:
Evidence presented in the medical literature to date indicates that while local anesthesia has risks… the dangers of general anesthesia are more impressive. I have performed or supervised over 10,000 abortions from 6 through 24 menstrual weeks' gestation under local anesthesia without a single serious anesthetic reaction; therefore I doubt whether there is any justification, other than uncontrolled epilepsy or agitated psychosis, for the use of general anesthesia in abortion. Patient comfort and physician convenience appear to be highly marginal indications for general anesthesia considering the risks involved. The degree of bleeding experienced under general anesthesia is greater, the risk of perforation is greater, and the risk of death due to aspiration of vomitus, among other things, appears to be greater. I believe it is preferable to have a patient who is uncomfortable but able to tell me what she is feeling and if she feels a strange new abdominal pain than to have a patient who is quite comfortable because she is dead.9

TOOLS OF MASS DESTRUCTION. Clockwise from top left: speculum, tenaculum, syringe, forceps, mayo scissors, manual vacuum aspirator, curette, cannula, and dilators.
Click here to share this design online. Click here to buy the T-shirt.
Prior to the administration of local anesthesia, a speculum is inserted into the vagina, and the blades are opened to allow the abortionist to visualize the cervix. In most cases, a local anesthetic is injected into the lip of the cervix and a tenaculum is used to position the cervix for full paracervical anesthesia10—generally consisting of four injections.11 The deeper the injections, the more effective the anesthesia. Next comes dilation. Unless the cervix is dilated, it is impossible to gain access to the uterus. Most North American abortionists dilate the cervix mechanically using tapered dilators.12 The NAF warns that "forcible dilation of a noncompliant cervix can result in lacerations or perforations."13
Once a cervical opening of sufficient size is achieved, a rigid or plastic cannula is inserted. Generally speaking, the size of the cannula coincides with the gestational age of the embryo or fetus.14 A 7-mm cannula would be used at 7-weeks gestation. It should be noted that gestational age does not reflect the actual age of the embryo or fetus. It is roughly two weeks ahead. As explained by the NAF, "In contrast to embryologists who describe pregnancy events from the time of fertilization, clinicians typically date pregnancy from the first day of the last menstrual period (LMP)."15 As such, an embryo that is aged 7-weeks gestation is actually 5-weeks from fertilization. The NAF reports that while it's possible for a 16-mm suction cannula to remove a fetus of 16 weeks' size, "forceps may be needed to extract some fetal parts such as the calvarium (skull) or spine."16 In actual practice, suction curettage is almost never performed after 12-weeks gestation.
Warren Hern's textbook on abortion advises against performing a surgical abortion prior to 7-weeks gestation. He believes that "the risks of complications in the very early pregnancy terminations (4-6 weeks from LMP) outweigh the benefits"17—namely the increased risk of an undiagnosed, incomplete abortion. More recently, advances in pregnancy testing, transvaginal ultrasound, and the advent of smaller, plastic cannulae have increased the frequency of earlier, surgical abortions,18 though the likelihood of a continuing pregnancy is still higher for abortions performed prior to 7-weeks gestation.19 The percentage of U.S. clinics offering abortion at 4-weeks LMP rose from 7% in 1993 to 40% in 2005.20
After the cannula is inserted into the uterus, the other end is attached to the tubing of an aspirator. The aspirator provides the necessary suction to empty the uterus, pulling the developing human being to pieces in the process. The cannula is rotated side to side, from the back of the uterus to the front until the "flow of tissue through the cannula and hose ceases."21 Only an estimated 21% of North American abortionists routinely use intraoperative ultrasound to guide them through a first-trimester aspiration abortion, despite its much lower rate of complication.22 By contrast, 91% routinely perform ultrasound prior to a first-trimester aspiration abortion as a means of confirming pregnancy gestation.23
About half of all suction abortions in the United States are performed with a manual vacuum aspirator (MVA).24 The rest are performed with an electric aspirator. The NAF reports that though there is no clear gestational age limit for MVAs, it is rarely used after 9 weeks' gestation since the MVA must be emptied multiple times per abortion.25 Because the force of suction is less severe with an MVA, it is easier to identify the embryo and placenta after the abortion, "due to less tissue shredding."26 This helps facilitate tissue examination, which is necessary to confirm a complete abortion. As revealed by the NAF, "Very small embryo-fetal parts may be apparent at 9 weeks' gestations and become easier to identify thereafter."27 The NAF lists "the ease and speed of uterine evacuation" and "more intact tissue (to facilities gross examination)" among the advantages of using a larger cannula. The advantage of a smaller cannula is less discomfort to the aborting woman.28 The NAF further reveals that "when cervical dilation is snug, placental tissue or, in later gestations, the calvarium (skull) may have difficulty passing through the cannula.29 If body parts are too large to pass, the NAF instructs the abortionist to "use a ring forceps to remove any material that is wedged in the end of the cannula or lodged at the external os."30 About 50% of North American abortionists perform sharp curettage after suctioning to confirm complete evacuation, scraping the lining of the uterus with a metal curette.31
Warren Hern describes his post-abortion procedure this way:
As the physician completes the procedure, he should inform the patient that the procedure is being completed… Keeping the vaginal bimanual examination hand sterile, the physician removes the speculum with the other gloved hand and proceeds to conduct a postoperative bimanual examination. If the uterine size seems larger than expected, the physician should replace the speculum and determine whether, in fact, the procedure has not been completed… As I complete the bimanual examination, I ask each patient to place the fingertips of both her hands over the uterus and rub constantly for 2 hours… this will help the uterus to contract and thereby stop the bleeding and cramps.32
After the bimanual examination is complete, Hern moves around to the side of the table and reassures the woman that "she is no longer pregnant." According to Hern, many of them cry.33 Statistically, suction abortion does fatal harm to an innocent human being 98 to 99.7% of the time.34
Early Medical Abortion:
Mifepristone, sometimes known as RU486, is the name of the abortion drug developed in the early 1980's by French bio-chemist, Etienne-Emile Baulieu.35 It works by prohibiting the synthesis and functionality of progesterone, a hormone that is necessary to sustain early pregnancy. When the role of progesterone is compromised, the uterus contracts, the endometrium becomes hostile to the implanted embryo, and the cervix softens to allow expulsion.36
Active testing on mifepristone began in 1982. After it was determined that mifepristone alone was no more than 80% effective at inducing abortion, a prostaglandin analog was added to the regimen. The use of mifepristone was first licensed in France and China in 1988.37 By 1998, most European countries had followed suit. The sale and use of mifepristone was not approved in the United States until 2001. By 2015, approximately 27% of all U.S. abortions were being performed medically.38 The percentage of medical abortion by state varies from 0 to 55% of all abortions.39
Medical abortion is often sold as a less-invasive, more-natural procedure than surgical abortion, though the National Abortion Federation (NAF) emphasizes the fact that there is no moral distinction between medical abortion and surgical abortion. They write:
Some patients report that they prefer the medical abortion because it seems like a heavy period or a miscarriage rather than an abortion… It is important for the patient's postabortion well-being that she does not fool herself (into thinking she is not having an abortion) and that the provider does not participate in her self-deception.40
The NAF further points out that, due to the risk of teratogenicity,41 any woman who undergoes a medical abortion must also consent to undergoing a surgical abortion should the medical procedure fail.42 According to the NAF, women who choose medical abortion "like that it is noninvasive and offers more privacy and control," while those who choose surgical abortion do so "because it is quick, predictable, and may be combined with sedation or anesthesia."43 In contrast to surgical abortion, women who abort medically experience the passage of their embryo firsthand. NAF physicians are encouraged to explain that though the conceptus is very small and is often obscured by blood clots, patients may still see a recognizable body.44 The NAF suggests showing women true-to-size illustrations of the "products of conception" as a way of preparing them for this potential trauma.45
The standard, clinical application of mifepristone requires three visits. During the first visit, the mother's consent is obtained and the age of her embryo is determined. The use of mifepristone is generally only approved through 49 days' gestation.46 In the United States, ultrasound is routinely used to verify fetal age. After the embryo's age is verified, mifepristone is taken orally, in the presence of the abortionist, by way of three 200-mg pills. The second visit happens 36 to 48 hours after the mifepristone was administered. Less than 5% of women expel the embryo prior to the second visit.47 For those still pregnant, a prostaglandin analog (generally misoprostol) is taken in the form of two 200 µg tablets. Women generally remain at the clinic for up to four hours. If four hours pass without expulsion, an examination is performed before discharge, to see if the gestational sac is trapped in the vagina. The first large-scale clinical trial of this regimen in the U.S. indicated that 49% of women abort within four hours of misoprostol administration and 75% abort within 24 hours; the median duration of bleeding is 13 days.48 The third visit happens two weeks later, and if the abortion has yet to be confirmed, a sonographic examination takes place. If the mother is still pregnant, a vacuum aspiration abortion is scheduled.
Statistically, early medical abortion does fatal harm to an innocent human being 94.8 to 97.6% of the time.49
Dilation and Evacuation (D&E) Abortion:
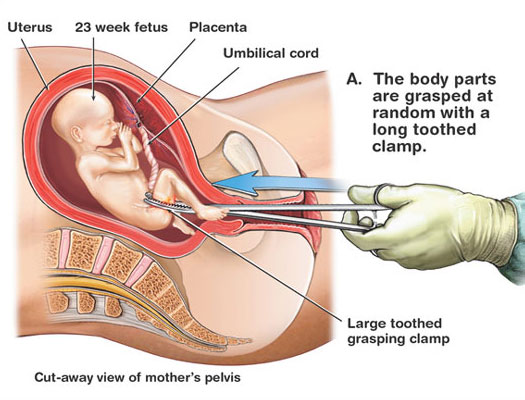
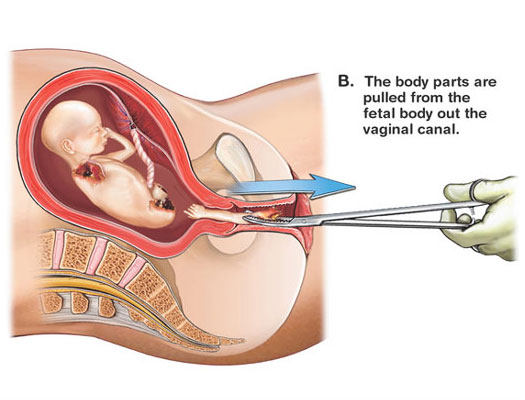
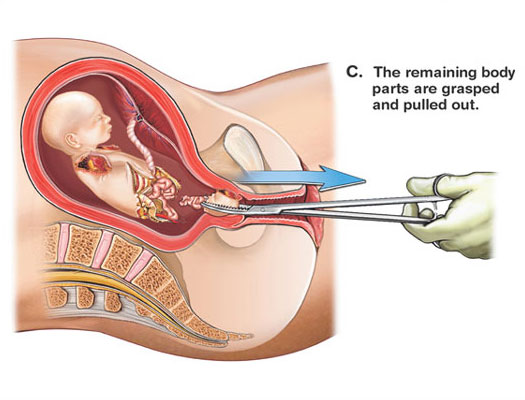
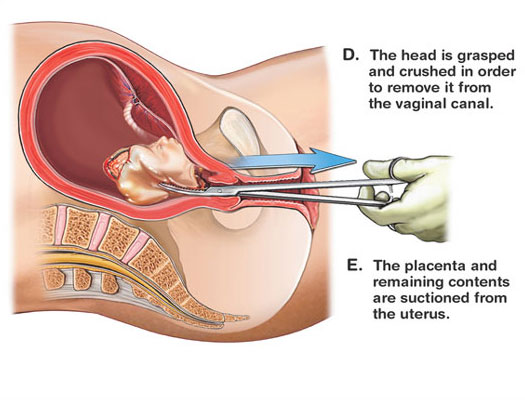
MEDICAL ILLUSTRATIONS OF A D&E ABORTION (click images to enlarge)
Copyright © Nucleus Medical Art, Inc. All rights reserved. www.nucleusinc.com
Around the globe, 10 to 15% of all abortions occur after the first trimester.50 In the United States, roughly 12% occur after 12 weeks' gestation; 3.8% of U.S. abortions occur between 16 and 20 weeks gestation while 1.4% occur after 20 weeks.51 These percentages have varied little since 1992. Ninety-six percent of all second-trimester U.S. abortions are performed by dilation and evacuation (D&E)–up from 31% in 1974.52 The National Abortion Federation (NAF) reports that most women seeking second-trimester abortion are young and healthy.53 Serious health problems account for only a small proportion of abortions worldwide.54 According to the NAF, the most common reasons for a second-trimester abortion include a delay in recognizing or admitting pregnancy, difficulty obtaining funds for an abortion, indecision over what to do, or changed circumstances.55 Circumstantial changes might include abandonment by their partner or the realization that they are carrying a girl instead of a boy. The NAF counsels that though "some abortion care providers may find it difficult to accept sex selection as a valid reason for an abortion," they should yield to the moral judgment of the patient who may believe that "aborting a female fetus is a rational act for the future good of the family."56 Globally, "the 10 to 15% of all abortions that take place after the first trimester cause approximately two-thirds of all major complications and half of all abortion-related maternal deaths."57
In a D&E abortion, patients generally undergo 1 to 2 days of preoperative cervical dilation. The NAF writes that the fundamental, historical challenge to transvaginal surgical abortion was the difficulty in finding "an atraumatic means to dilate the uterine cervix that would permit successful extraction of the enlarging second-trimester fetus."58Though osmotic dilation techniques using processed seaweed tents (laminaria) were common in Japan and Eastern Europe, they didn't make their way to the United States until the early 1970's.59 Laminaria come in at least 11 diameters ranging from 2 to 10 mm. As the laminaria absorb fluid, they swell to three or four times their dry width, without increasing in length. Direct radial pressure against the surrounding cervical stroma gradually dilates the cervix. The amount of dilation required depends on the gestational age and size of the fetus being aborted. Laminaria are placed by grasping the cervix with a single-tooth tenaculum and using forceps to insert the laminaria into the endocervical canal.60
The surgical portion of a D&E abortion begins with the insertion of the speculum. "Late in the second trimester," the NAF notes, "a weighted speculum accommodates larger fetal parts and allows more angulation of the forceps."61 Throughout the procedure, "strong and steady traction" on the cervix must be maintained with a tenaculum.62 This allows forceps to be inserted through the dilated cervix for the dismemberment and removal of the human fetus. Ring forceps require a minimal cervical dilation of 10-12 mm, but are not sufficient for gestations beyond 17 to 18 weeks, when longer and weightier forceps must be used. The NAF reports that "Bierer forceps are the weightiest and largest-jawed [with] fenestrated and sharply serrated jaws (to) provide the most traction."63 The NAF recommends that ultrasound guidance be used "in cases that require a considerable degree of force to remove fetal parts."64 This helps ensure that the abortionist does not accidentally grasp and tear the myometrium (uterine wall) while grasping and tearing apart the fetus.
The National Abortion Federation instructions for a D&E abortion are as follows:
Once the forceps has passed through the internal os, open the jaws as widely as possible to encircle the fetal tissue and avoid pushing fetal parts deeper into the fundus… After 16 weeks' gestation, fetal skeletal development is such that the surgeon can manually sense the presence of fetal parts within the closed jaws… After grasping a fetal part, withdraw the forceps while gently rotating it. This maneuver brings the fetus into the lower uterine segment before the grasped fetal part is separated (if necessary) and removed from the cervix… If a fetal extremity is brought through the cervix without separation, advance the forceps beyond the extremity to grasp part of the fetal trunk. Bringing the fetal trunk into the lower segment markedly reduces the number of instrument passes into the fundus… During the procedure, try to identify and keep track of fetal parts as they are removed. A "pouch' or surgical pan at the edge of the gable to catch fetal parts can assist this process.65
Warren Hern, who the NAF credits as being an "American innovator"66 in D&E technique, offers the following instruction:
It is better to use smaller forceps and take smaller amounts of tissue each time than to deliver fetal parts intact while traumatizing the cervix… At 16 to 17 weeks, fetal tissue is much more easily identifiable with the forceps and in some ways is easier to grasp and remove than in earlier gestations. The [skull] is about the size of a Ping-Pong ball and usually can be grasped readily with the Bierer. Collapsing it gives a definite sensation… At 18-19 menstrual weeks… fetal parts are significantly larger and more difficult to morcellate (tear into pieces)… [Abortion after the] 20-week gestation… can be a significantly more difficult procedure accompanied by unnerving hemorrhage. Forceps use must be sure and relatively rapid. There is frequently not much time for exploring the nuances of different tissue sensations. Grasping and collapsing the [skull is] often difficult. Stripping the [skull] of soft tissue is sometimes the first step in successful delivery of this part, followed by dislocation of parietal bones. In this case, care must be taken in removal because ossification is occurring and the edges are sharp… Regardless of the amount of dilatation, delivery of the [skull] and pelvis is sometimes difficult… The advantage obtained by having a softened cervix could become a disaster if a laceration develops at the level of the internal os as the result of too much force… The procedure changes significantly at 21 weeks because the fetal tissues become much more cohesive and difficult to dismember. This problem is accentuated by the fact that the fetal pelvis may be as much as 5 cm in width… [The skull] can be collapsed. Other structures, such as the pelvis, present more difficulty… A long curved Mayo scissors may be necessary to decapitate and dismember the fetus, since it may be impossible to apply forceps or to do so while avoiding the thinned-out cervix."67
After the abortion takes place, fetal parts must be examined "to verify complete evacuation."68 A foot of the aborted fetus is often measured to "estimate gestational age after abortion."69 Postoperative observation lasts for an hour or more so that the patient can be observed for "bleeding or pain that may signal uterine atony, retained tissue, disseminated intravascular coagulopathy, or uterine perforation."70 Statistically, dilation and evacuation does fatal harm to an innocent human being virtually 100% of the time.
Dilation and Extraction (D&X) or Partial Birth Abortion:
Dilation and Extraction (D&X) is a variant of dilation and evacuation (D&E) whereby the aborted fetus is delivered intact instead of in pieces. Politically, it is known as partial-birth abortion. In the United States, this particular method of abortion was federally banned in 2003, after passage of the Partial-Birth Abortion Ban Act. The ban was upheld by the Supreme Court in 2007 in Gonzales v. Carhart. As the name implies, the fatal action of partial-birth abortion does not occur until a portion of the baby has passed through the cervix. The National Abortion Federation (NAF) describes the procedure this way:
Because the cranium represents the largest and least compressible structure, it often requires decompression… Decompression can be accomplished with forceps or by making an incision at he base of the skull through which the intracranial contents are suctioned. If the fetus is in cephalic presentation (head first) with the calvarium well-applied to the cervix, the surgeon can pierce the calvarium with a sharp instrument and collapse it externally.71
In lay terms, if the baby is delivered feet first, the head is crushed with forceps or pierced with scissors (allowing the brain to be suctioned out by vacuum aspiration). If the baby is delivered head first, scissors are used to pierce the top of the head as soon as it appears at the cervical opening. To position the baby in a D&X abortion, the NAF recommends using Hern forceps. They have "fewer and smaller teeth"–which are "especially useful when traction or rotation of an intact fetus is desired (instead of dismemberment)."72 Warren Hern, who developed the Hern forceps, writes this in Abortion Practice:
Cervical obstruction by the calvaria (skull) is a paradoxical problem, since it is the opposite of having difficulty in recovering tissue… Small instruments cannot encompass it; large instruments… either push it away, cannot be closed once the [skull] is grasped, or, having grasped the [skull], cannot be withdrawn. Unless the [skull] can be collapsed and delivered, however, the procedure cannot be completed… and the risk of complications begin to increase. The most useful maneuver in this case is to grasp the presenting of the [skull] with the cervical tenaculum, stripping away the soft tissue (skin). When the skull bones are visible, they are grasped also with the tenaculum. A long curved Mayo scissors is then used to dissect the [skull] to the point that it is opened and decompressed. At this time, a forceps with a very strong blade and firm grasp… may be used to grasp the tentorium and skull plates, sometimes dismembering by torsion and sometimes by sharp dissection with the Mayo (scissors)… Once some dismemberment has taken place, the operator may take a somewhat larger forceps… As the tissue is pushed slightly up in to the uterine cavity, the forceps blade is opened and a moderate amount of tissue is grasped… With good dilatation and effacement, the entire fetus may be delivered.73
According to the language of the Partial Birth Abortion Ban Act of 2003, "punctur[ing] the back of [a] child's skull with a Sharp instrument, and suck[ing] the child's brains out before completing delivery of the dead infant -- is a gruesome and inhumane procedure that is never medically necessary and should be prohibited."74 The subsequent Supreme Court ruling held that those challenging the constitutionality of the Act were not able to demonstrate that the Act was "void for vagueness, or that it impose[d] an undue burden on a woman’s right to abortion based on its overbreadth or lack of a health exception."75 What is most perplexing about the 2003 ban is not the assertion that partial-birth abortion is "gruesome and inhumane," but the implication that it is more gruesome and inhumane than other abortion methods. The syllabus of Gonzales v. Carhart describes the difference between "usual" D&E technique and "intact D&E" this way:
In the usual second-trimester procedure, “dilation and evacuation” (D&E), the doctor dilates the cervix and then inserts surgical instruments into the uterus and maneuvers them to grab the fetus and pull it back through the cervix and vagina. The fetus is usually ripped apart as it is removed, and the doctor may take 10 to 15 passes to remove it in its entirety. The procedure that prompted the federal Act and various state statutes, including Nebraska’s, is a variation of the standard D&E, and is herein referred to as “intact D&E.” The main difference between the two procedures is that in intact D&E a doctor extracts the fetus intact or largely intact with only a few passes, pulling out its entire body instead of ripping it apart. In order to allow the head to pass through the cervix, the doctor typically pierces or crushes the skull.76
In an objective analysis of the two procedures, there is no obvious reason for declaring D&X to be more gruesome and inhumane than D&E. Strictly speaking, D&X is the less violent of the two. The NAF condemns both Congress and the Supreme Court for "denying reproductive freedom"77 and "ignor[ing] the best judgment of the medical community."78 Included among their reasons for why D&X can be more advantageous than D&E is the assertion that it "permit(s) more complete morphologic evaluation of an extracted fetus,"79 it "minimizes the risk of retained tissue,"80 and it gives grieving parents "the opportunity to view or hold an intact fetus."81
To circumvent the Partial-Birth Abortion Ban, the NAF advises abortionists to kill the baby by injection prior to performing a D&X procedure. According to the language of the Ban, it is "applicable only when a 'living fetus' is present at the outset of evacuation."82 The NAF offers the following advice for killing babies by injection:
Digoxin in doses of 1.0 to 1.5 mg appears to effect fetal demise. Providers may feel a change in resistance at the needle tip as it enters the fetus. Unless the needle is in the fetal cardiac chambers, aspiration will not usually yield fetal blood… fetal demise occurred in 43% at 2 hours; 75% at 3 hours , and 98% in 5 hours… Potassium chloride will not achieve fetal demise when injected into the amniotic fluid; injection into the fetal heart or umbilical cord is required… Needle placement should be maintained until fetal death is confirmed monographically. These technically challenging procedures are performed most commonly for multifetal pregnancy reduction… Clinicians typically administer agents to cause fetal demise 1 to 2 days before D&E, often in conjunction with cervical preparation.83
The NAF concludes that "published data confer no clear medical benefit of causing fetal demise (by injection), although individual practitioners may want to consider it if: (1) in their experience fetal cortical bone softening makes the procedure easier; (2) a patient expresses a preference for fetal death prior to operative evacuation; (3) they desire to avoid the possibility of unscheduled delivery of a live fetus; or (4) they are concerned about compliance with the Partial-Birth Abortion Ban Act of 2003."84 Elsewhere, the NAF warns that euthanizing a baby born alive "may have legal implications."85 Apparently, the only thing that would compel an abortionist not to euthanize a baby that was born alive after a failed abortion is legal prohibition.
Statistically, dilation and extraction does fatal harm to an innocent human being virtually 100% of the time.
This page was last updated on May 24, 2019. To cite this page in a research paper, visit: "Citing Abort73 as a Source."
- Warren M. Hern. Abortion Practice (Philadelphia: J.B. Lippincott Company, 1990), 101.
- Karen Meckstroth MD, MPH, and Maureen Paul MD, MPH, “First-Trimester Aspiration Abortion,” Management of Unintended and Abnormal Pregnancy. Ed. Paul, Lichtenberg, Borgatta, Grimes, Stubblefield and Creinin. (Wiley-Blackwell, 2009), 135.
- Ibid, 136.
- Ibid, 135.
- Tara C. Jatlaoui, MD, et al, “Abortion Surveillance—- United States, 2015,” Morbidity and Mortality Weekly Report (MMWR). (Centers for Disease Control and Prevention, Nov 23, 2018), Table 11.
- Ibid.
- Anne Baker, MA and Terry Beresford, BA, “Informed Consent, Patient Education, and Counseling,” Management of Unintended and Abnormal Pregnancy. Ed. Paul, Lichtenberg, Borgatta, Grimes, Stubblefield and Creinin. (Wiley-Blackwell, 2009), 59.
- Mark Nichols MD, et al, “Pain Management,” Management of Unintended and Abnormal Pregnancy. Ed. Paul, Lichtenberg, Borgatta, Grimes, Stubblefield and Creinin. (Wiley-Blackwell, 2009), 92.
- Warren M. Hern. Abortion Practice (Philadelphia: J.B. Lippincott Company, 1990), 119.
- Mark Nichols MD, et al, “Pain Management,” Management of Unintended and Abnormal Pregnancy. Ed. Paul, Lichtenberg, Borgatta, Grimes, Stubblefield and Creinin. (Wiley-Blackwell, 2009), 93.
- Ibid, 94.
- Karen Meckstroth MD, MPH, and Maureen Paul MD, MPH, “First-Trimester Aspiration Abortion,” Management of Unintended and Abnormal Pregnancy. Ed. Paul, Lichtenberg, Borgatta, Grimes, Stubblefield and Creinin. (Wiley-Blackwell, 2009), 138.
- Ibid, 145.
- Ibid.
- Steven R. Goldstein, MD and Matthew F. Reeves, MD, MPH, “Clinical Assessment and Ultrasound in Early Pregnancy,” Management of Unintended and Abnormal Pregnancy. Ed. Paul, Lichtenberg, Borgatta, Grimes, Stubblefield and Creinin. (Wiley-Blackwell, 2009), 63.
- Cassing Hammond MD, and Stephen Chasen MD, “Dilation and Evacuation,” Management of Unintended and Abnormal Pregnancy. Ed. Paul, Lichtenberg, Borgatta, Grimes, Stubblefield and Creinin. (Wiley-Blackwell, 2009), 171.
- Warren M. Hern. Abortion Practice (Philadelphia: J.B. Lippincott Company, 1990), 120.
- Karen Meckstroth MD, MPH, and Maureen Paul MD, MPH, “First-Trimester Aspiration Abortion,” Management of Unintended and Abnormal Pregnancy. Ed. Paul, Lichtenberg, Borgatta, Grimes, Stubblefield and Creinin. (Wiley-Blackwell, 2009), 135, 148.
- 19 Ibid, 148.
- 20 Ibid.
- Ibid, 146
- Ibid, 148.
- Ibid, 138.
- Ibid, 141.
- Ibid.
- Laura Castleman MD, MPH, MBA, et al, “Providing Abortion in Low-Resource Settings,” Management of Unintended and Abnormal Pregnancy. Ed. Paul, Lichtenberg, Borgatta, Grimes, Stubblefield and Creinin. (Wiley-Blackwell, 2009), 323.
- Karen Meckstroth MD, MPH, and Maureen Paul MD, MPH, “First-Trimester Aspiration Abortion,” Management of Unintended and Abnormal Pregnancy. Ed. Paul, Lichtenberg, Borgatta, Grimes, Stubblefield and Creinin. (Wiley-Blackwell, 2009), 149.
- Ibid, 147.
- Ibid, 143.
- Ibid, 146.
- Ibid, 148.
- Warren M. Hern. Abortion Practice (Philadelphia: J.B. Lippincott Company, 1990), 162.
- Ibid.
- E. Steve Lichtenberg MD, MPH, and David A. Grimes MD, “Surgical Complications: Prevention and Management,” Management of Unintended and Abnormal Pregnancy. Ed. Paul, Lichtenberg, Borgatta, Grimes, Stubblefield and Creinin. (Wiley-Blackwell, 2009), 228.
- Mitchell D. Creinin MD, and Kristina Gemzell Danielsson MD, PhD, “Medical Abortion in Early Pregnancy,” Management of Unintended and Abnormal Pregnancy. Ed. Paul, Lichtenberg, Borgatta, Grimes, Stubblefield and Creinin. (Wiley-Blackwell, 2009), 112.
- Ibid, 113.
- Ibid, 112.
- Tara C. Jatlaoui, MD, et al, “Abortion Surveillance—- United States, 2015,” Morbidity and Mortality Weekly Report (MMWR). (Centers for Disease Control and Prevention, Nov 23, 2018).
- Ibid, Table 11.
- Steven R. Goldstein, MD and Matthew F. Reeves, MD, MPH, “Clinical Assessment and Ultrasound in Early Pregnancy,” Management of Unintended and Abnormal Pregnancy. Ed. Paul, Lichtenberg, Borgatta, Grimes, Stubblefield and Creinin. (Wiley-Blackwell, 2009), 60.
- Mitchell D. Creinin MD, and Kristina Gemzell Danielsson MD, PhD, “Medical Abortion in Early Pregnancy,” Management of Unintended and Abnormal Pregnancy. Ed. Paul, Lichtenberg, Borgatta, Grimes, Stubblefield and Creinin. (Wiley-Blackwell, 2009), 123.
- Steven R. Goldstein, MD and Matthew F. Reeves, MD, MPH, “Clinical Assessment and Ultrasound in Early Pregnancy,” Management of Unintended and Abnormal Pregnancy. Ed. Paul, Lichtenberg, Borgatta, Grimes, Stubblefield and Creinin. (Wiley-Blackwell, 2009), 60.
- Karen Meckstroth MD, MPH, and Maureen Paul MD, MPH, “First-Trimester Aspiration Abortion,” Management of Unintended and Abnormal Pregnancy. Ed. Paul, Lichtenberg, Borgatta, Grimes, Stubblefield and Creinin. (Wiley-Blackwell, 2009), 137.
- Mitchell D. Creinin MD, and Kristina Gemzell Danielsson MD, PhD, “Medical Abortion in Early Pregnancy,” Management of Unintended and Abnormal Pregnancy. Ed. Paul, Lichtenberg, Borgatta, Grimes, Stubblefield and Creinin. (Wiley-Blackwell, 2009), 124.
- Ibid.
- Ibid, 116.
- Ibid.
- Ibid.
- Ibid.
- Cassing Hammond MD, and Stephen Chasen MD, “Dilation and Evacuation,” Management of Unintended and Abnormal Pregnancy. Ed. Paul, Lichtenberg, Borgatta, Grimes, Stubblefield and Creinin. (Wiley-Blackwell, 2009), 179.
- Ibid, 157.
- Ibid, 158.
- Ibid, 159.
- Jeffrey S. Dugan MD and Lee P. Shulman MD, “Abortion for Fetal Abnormalities or Maternal Conditions,” Management of Unintended and Abnormal Pregnancy. Ed. Paul, Lichtenberg, Borgatta, Grimes, Stubblefield and Creinin. (Wiley-Blackwell, 2009), 302.
- Cassing Hammond MD, and Stephen Chasen MD, “Dilation and Evacuation,” Management of Unintended and Abnormal Pregnancy. Ed. Paul, Lichtenberg, Borgatta, Grimes, Stubblefield and Creinin. (Wiley-Blackwell, 2009), 179.
- Anne Baker, MA and Terry Beresford, BA, “Informed Consent, Patient Education, and Counseling,” Management of Unintended and Abnormal Pregnancy. Ed. Paul, Lichtenberg, Borgatta, Grimes, Stubblefield and Creinin. (Wiley-Blackwell, 2009), 60.
- Laura Castleman MD, MPH, MBA, et al, “Providing Abortion in Low-Resource Settings,” Management of Unintended and Abnormal Pregnancy. Ed. Paul, Lichtenberg, Borgatta, Grimes, Stubblefield and Creinin. (Wiley-Blackwell, 2009), 324.
- Cassing Hammond MD, and Stephen Chasen MD, “Dilation and Evacuation,” Management of Unintended and Abnormal Pregnancy. Ed. Paul, Lichtenberg, Borgatta, Grimes, Stubblefield and Creinin. (Wiley-Blackwell, 2009), 157.
- Ibid, 158.
- Ibid, 161.
- Ibid, 169.
- Ibid.
- Ibid, 170.
- Ibid, 171.
- Ibid, 172.
- Ibid, 158.
- Warren M. Hern. Abortion Practice (Philadelphia: J.B. Lippincott Company, 1990), 150-154.
- Cassing Hammond MD, and Stephen Chasen MD, “Dilation and Evacuation,” Management of Unintended and Abnormal Pregnancy. Ed. Paul, Lichtenberg, Borgatta, Grimes, Stubblefield and Creinin. (Wiley-Blackwell, 2009), 173.
- Ibid.
- Ibid, 174.
- Cassing Hammond MD, and Stephen Chasen MD, “Dilation and Evacuation,” Management of Unintended and Abnormal Pregnancy. Ed. Paul, Lichtenberg, Borgatta, Grimes, Stubblefield and Creinin. (Wiley-Blackwell, 2009), 173.
- Ibid, 170.
- Warren M. Hern. Abortion Practice (Philadelphia: J.B. Lippincott Company, 1990), 199-200.
- Partial Birth Abortion Ban Act of 2003. United States Congress, 108th Congress, 1st Session (http://news.findlaw.com/wsj/docs/abortion/2003s3.html).
- Gonzales, Attorney General v. Carhart et al (Nos. 05-380 and 05-1382). Supreme Court of the United States. Argued November 8, 2006—Decided April 18, 2007 (http://www.law.cornell.edu/supct/html/05-380.ZS.html) Syllabus.
- Ibid.
- Allan Rosenfield MD, “Foreword,” Management of Unintended and Abnormal Pregnancy. Ed. Paul, Lichtenberg, Borgatta, Grimes, Stubblefield and Creinin. (Wiley-Blackwell, 2009), xi.
- Carole Joffe, PhD, “Abortion and Medicine: A Sociopolitical History,” Management of Unintended and Abnormal Pregnancy. Ed. Paul, Lichtenberg, Borgatta, Grimes, Stubblefield and Creinin. (Wiley-Blackwell, 2009), 5.
- Cassing Hammond MD, and Stephen Chasen MD, “Dilation and Evacuation,” Management of Unintended and Abnormal Pregnancy. Ed. Paul, Lichtenberg, Borgatta, Grimes, Stubblefield and Creinin. (Wiley-Blackwell, 2009), 159.
- Ibid, 173.
- Ibid.
- Ibid, 166.
- Ibid, 167.
- Ibid, 169.
- Nathalie Kapp MD, MPH, and Helena von Hertzen MD, DDS, “Medical Methods to Induce Abortion in the Second Trimester,” Management of Unintended and Abnormal Pregnancy. Ed. Paul, Lichtenberg, Borgatta, Grimes, Stubblefield and Creinin. (Wiley-Blackwell, 2009), 180.
Footnotes
Possible Objection:
Though abortion procedures are not pleasant, abortion is a far better solution than for an unwanted child to be born into a life of neglect. It mercifully spares them a great deal of suffering.
To learn our response, continue to the next page: Abortion Pictures
Related Entries:
- Abortion and the Hippocratic Oath: The original rendering of this historic creed explicitly condemns abortion.
- Do Unborn Children Feel Pain?: Abortion may or may not be painful for the fetus, but it is always fatal.
- Is Abortion Painful for Women?: Pain is relative, but many women do find abortion to be physically painful.
For Further Study:
- The Grantham Collection Abortion Instruments Archive
- The Absurdity of Banning Partial-Birth Abortion (Abort73 Blog)
- Doctor or Abortionist? (Abort73 Blog)
- Transvaginal Ultrasound and the Fallacy of Control (Abort73 Blog)
- Life and Death: Comparing the Relative Safety of Abortion and Childbirth (Abort73 Blog)